Why health advice doesn’t stick — and what oral health can teach us about making habits easier
Health advice doesn’t fail because people don’t care. It fails because real life creates friction. Here’s what oral health can teach us about designing habits that actually stick — with clearer priorities, better prompts, and more supportive systems.
January is peak “new habits” season.
And yet, every year, many of those habits quietly fade — not because people don’t care, but because real life gets in the way.
In oral health, I see this all the time.
I’m Colette — a UK-based dental clinician and medical writer — and I spend a lot of time thinking about the overlap between oral health, prevention, and the systems (and tech) that make healthy habits easier to stick to.
Because advice can be clinically spot-on… and still not stick.
In clinic, it’s often clear that knowledge isn’t the missing piece. Many patients already know the basics: brush twice a day, clean between teeth, watch the sugar.
And yet, a patient said to me recently:
“I know what I’m meant to do… I just don’t manage it.”
That gap — between knowing and doing — is where prevention often breaks down.
And it’s why motivation alone is rarely the answer.
Why health advice doesn’t stick (even when it’s correct)
Most oral health (and general health) advice is well-intentioned and evidence-based.
But behaviour doesn’t happen in ideal conditions. It happens on busy mornings, late nights, shift patterns, school runs, sensory overload days, anxious days, and the “I’ve got nothing left in the tank” days.
So when habits slip, it’s rarely because someone doesn’t care.
More often, it’s because the habit sits behind too much friction.
Common reasons health habits fail (the friction points)
Too much complexity
Too many products, too many claims, too many “rules”. When people feel confused, they often do nothing.
No clear priority
If everything sounds equally important, it’s hard to know what matters today.
Timing
Advice is often given at a moment when people can’t act. The moment passes, and life takes over.
Shame and self-judgement
If someone feels they’ve already “failed”, they avoid the topic altogether. Shame doesn’t build habits — it blocks them.
Life factors that don’t get acknowledged
Neurodivergence, anxiety, depression, medication-related dry mouth, chronic illness, caring responsibilities, cost. These aren’t edge cases — they’re real life.
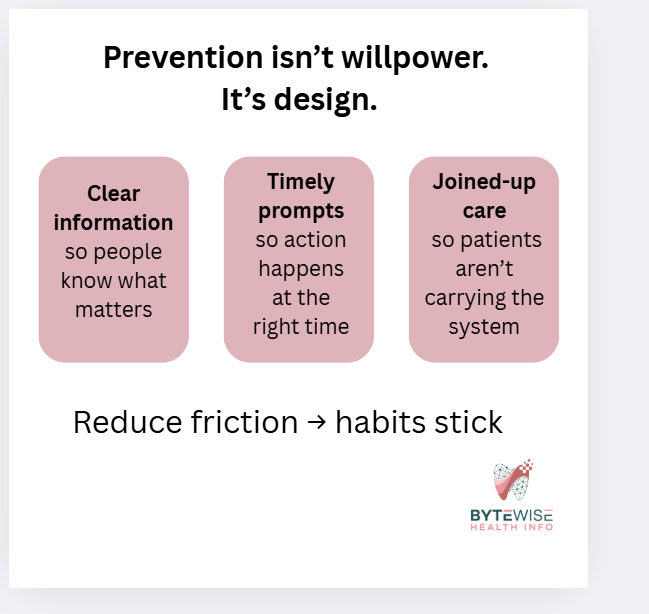
This is why I keep coming back to a simple idea:
Prevention is easier when the system is designed to support it — not with more pressure, but with better support.
Knowing vs doing: where prevention really lives
Most prevention challenges sit in the gap between:
Capability — Do I know how? Do I have the tools?
Opportunity — Is my environment set up to help me?
Motivation — Do I want to do this, and does it feel worth it?
We often focus heavily on motivation: try harder, be consistent.
But opportunity is frequently the missing piece — the prompts, routines, environment, and joined-up care that make follow-through more likely.
This is also where digital tools can help — including reminders, smart prompts, and in some cases wearables — as long as they’re designed around real human behaviour, not perfect routines.
What better systems (and tech) could do
This isn’t about fancy gadgets or downloading yet another app that gets abandoned by Thursday.
It’s about reducing friction and making prevention easier to repeat.
1. Personalised prevention, not one-size-fits-all
Oral health advice is often generic — but people aren’t.
Someone with dry mouth, braces, diabetes risk, previous gum disease, or high sugar exposure needs different support from someone who’s low risk.
Better systems could translate risk into clear, usable guidance like:
“Here are your top two priorities this month.”
“Here’s the one habit that will give you the biggest win.”
“Here’s what to focus on until your next visit.”
Clarity reduces overwhelm.
2. Prompts at the right moment (not random reminders)
Most reminders fail because they arrive when you can’t act.
More effective prompts show up at the point of decision — when a routine is already happening.
Even low-tech prompts work well:
linking interdental cleaning to an existing habit
keeping brushes or floss where you actually sit
a simple routine card on the bathroom mirror
recall messages sent during opening hours, when booking is easy
Tech can help with timing — but the goal is simple: make the next right action easier.
3. Joined-up records that support joined-up care
Oral health is linked to systemic health, medication, pregnancy, and chronic conditions — yet records are often siloed. This is something I explore further in my white paper on integrating dental and medical health records.
When data isn’t joined up, we rely on:
patients repeating their story
memory (not a safe clinical tool)
missed prevention opportunities
Better integration could flag:
diabetes risk and gum inflammation
medication-related dry mouth
anticoagulants and dental planning
osteoporosis medications
pregnancy-related inflammatory windows
This isn’t about “more data”.
It’s about the system doing some of the heavy lifting — so patients don’t have to.
4. Prevention that continues between appointments
Most people see a dental professional occasionally — but habits are daily.
Systems and tech could help bridge that gap with:
simple check-ins
consistent, non-judgemental encouragement
short, personalised “next step” nudges
easy access to the right education at the right time
Prevention works best when it feels supported, not like a once-a-year reset.
Three tiny friction-reducers to try this week
You don’t need a personality transplant. You need a simpler setup.
1. Put tools where the habit actually happens
Out of sight = out of routine. Move tools to where you intend to use them and leave them on show.
2. Attach the habit to something you already do
Borrow an existing routine so you don’t rely on memory.
3. Shrink the task
A “minimum version” still counts. Consistency beats perfection.
A quick note on shame
If you’ve ever felt embarrassed about your oral health routine, you’re not alone.
But shame doesn’t create good habits.
It creates avoidance.
Better systems support people — they don’t judge them.
Where I’m going with this in 2026
This year I’m leaning further into the systems side of prevention.
Not just what we tell people to do — but what actually helps people do it, consistently, in real life.
That includes:
clearer risk communication
better-timed prompts
joined-up records
and tech that supports habits without adding guilt
I’m also starting a behaviour change course to strengthen this side of my work — so my content is not only clinically accurate, but genuinely usable.
One last question
What’s the biggest thing that gets in the way of oral health habits sticking — for you, or for your patients?
Forgetfulness?
Time?
Anxiety or sensory issues?
Cost or access?
Medication or health factors?
Or just… life?
These real-world barriers are where better prevention design starts.
The Ultimate Guide to Choosing the Right Toothpaste
Choosing toothpaste shouldn’t feel overwhelming. This simple guide breaks down fluoride, hydroxyapatite, whitening pastes and SLS free options so you can choose the right toothpaste with confidence.
Choosing a toothpaste should be simple.
But walk down any supermarket aisle and it can suddenly feel like you need a degree in chemistry to understand what you are looking at.
"Whitening." "Enamel repair." "Nature identical minerals." "Ultra micro nano crystal technology."
The claims can be confusing, even when you do understand the science.
This guide breaks down the key toothpaste ingredients, what they actually do, and how to choose the best toothpaste for your needs in clear, normal human language.
The toothpaste aisle, decoded. A simple guide to ingredients and what they do.
How to Understand a Toothpaste Label
Fluoride – the essential one
Fluoride is the ingredient with the strongest, longest standing evidence for preventing tooth decay.
It helps to:
strengthen enamel
slow early decay
make teeth more resilient
This is why fluoride toothpaste is recommended for most adults.
You will usually see fluoride shown as ppm (parts per million). This simply describes the concentration of fluoride in the toothpaste.
Types of fluoride you will see
Most toothpastes use one of two main forms:
Sodium fluoride
Stannous fluoride
Both protect against decay.
Stannous fluoride also offers added benefits for gum health and sensitivity relief, which can make it a good choice for people with bleeding gums or sensitive teeth.
For everyday use, adults should choose toothpaste with 1,350 to 1,500 ppm fluoride.
How Much Fluoride Do Children Need?
For children, the recommended fluoride level and the amount of toothpaste used depends on their age:
Under 3 years: a smear of toothpaste with at least 1,000 ppm fluoride
Ages 3 to 6: a pea sized amount of 1,000 to 1,500 ppm
Age 7 and above: usually fine to use adult strength toothpaste (1,350 to 1,500 ppm)
Children often prefer milder flavours. It is absolutely fine to stay with a child friendly toothpaste as long as the fluoride level is appropriate.
When my three were younger, we often had several different tubes lined up on the bathroom shelf. One for each age and stage.
If your bathroom looks similar, you are not doing anything wrong. It is just a phase, and once everyone moves onto adult toothpaste, things get slightly simpler.
A note on how much toothpaste to use
Young children swallow toothpaste more often, and their adult teeth are still developing under the gums.
Using the right amount helps prevent fluorosis (a harmless but sometimes mottled appearance on enamel).
Under 3 years: a smear
Ages 3 to 6: a pea sized amount
A pea sized amount also makes it safe for children aged 3 and over to use adult strength toothpaste if needed, especially if they are more prone to decay.
If a child is at higher risk of tooth decay, your dentist or hygienist may recommend stronger fluoride toothpaste sooner, or prescribe a paste that is not available over the counter.
Hydroxyapatite toothpaste: what it does (and what to look for)
Hydroxyapatite is the mineral your enamel is made from, which is why it’s showing up in toothpaste. It’s a biomimetic (“nature-mimicking”) ingredient that supports enamel—often chosen by people who want a fluoride-free toothpaste. It isn’t a like-for-like replacement for fluoride, but it has its own role.
How hydroxyapatite works
Hydroxyapatite can help to:
“fill in” tiny surface defects on the enamel
reduce sensitivity
smooth the tooth surface
support remineralisation
For people looking for fluoride-free toothpaste, hydroxyapatite is one of the few ingredients with emerging evidence behind it.
Some toothpastes even combine fluoride and hydroxyapatite for a dual approach.
There is no standardised “ideal concentration” for hydroxyapatite yet. Brands are not always required to list the percentage. Some formulas use around 10 per cent, others vary.
Instead of focusing on a number, focus on:
choosing a reputable brand
checking that hydroxyapatite appears reasonably high on the ingredient list
Top tip:
If you spot words like “biomimetic”, “microcrystalline” or “nature identical mineral” on the packaging, it is often a marketing-friendly way of describing hydroxyapatite.
A Quick Note on Ingredient Sensitivities (Including During Chemotherapy)
Some people react to certain toothpaste ingredients.
Not with tooth sensitivity, but with irritation of the mouth tissues.
One of the most common triggers is SLS (sodium lauryl sulphate), a foaming agent found in many toothpastes.
SLS is considered safe, but for some people it can:
trigger mouth ulcers
cause a stinging or burning feeling
irritate the cheeks or lips
make the mouth feel drier
People undergoing chemotherapy can be especially sensitive to foaming agents and stronger flavours, because treatment often leaves the mouth dry, delicate, or more prone to ulceration.
If you notice toothpaste making your mouth feel sore, or if you are going through chemotherapy, switching to an SLS free, mild flavour toothpaste can make brushing far more comfortable.
Most brands clearly label “SLS free” on the front of the packaging.
If not, a quick check of the ingredient list on the back will tell you. You are looking for “Sodium Lauryl Sulphate” (or “Sodium Lauryl Sulfate” with the American spelling).
If it is not listed, the toothpaste is generally SLS free.
SLS free toothpastes clean just as effectively. They simply foam less.
Whitening Toothpaste – What Actually Works?
You have probably seen the promises:
“Instant whitening.”
“Five shades brighter.”
Some claims are hopeful. Some are pure sparkle. So what do whitening toothpastes actually do?
Mild abrasives – the stain polishers
Most whitening toothpastes use ingredients like hydrated silica to gently polish away surface stains from coffee, tea and red wine.
These are great for lifting daily staining, but they will not change the natural colour of your teeth.
Chemical lighteners – the gentle lifters
Some formulas contain low dose hydrogen peroxide or carbamide peroxide.
These can brighten the surface slightly, but they do not reach deeper pigments in the same way professional whitening gels do.
Optical brighteners – the illusionists
Some pastes use blue pigments (such as blue covarine) that temporarily change the way light reflects off enamel, giving an instant but short lived brightness boost.
What I see in practice
In day to day practice, the best “everyday brightening” results usually come from:
a mildly abrasive whitening toothpaste
used with an electric toothbrush
It will not transform your tooth shade, but it can noticeably lift surface staining.
A note on tooth sensitivity
Whitening toothpastes can increase tooth sensitivity, especially if they are more abrasive.
If your teeth tend to twinge:
try a whitening plus sensitivity toothpaste, or
alternate your whitening paste with a regular fluoride toothpaste
The Bottom Line – How to Choose the Right Toothpaste
Here is a quick summary to help you choose:
For cavity protection:
A fluoride toothpaste with 1,350 to 1,500 ppm fluorideFor sensitivity:
Toothpaste with stannous fluoride or potassium nitrateFor a more “natural” option:
Hydroxyapatite toothpaste from a reputable brandFor gum health:
Stannous fluoride or CPC (cetylpyridinium chloride)For whitening:
Mild abrasive whitening paste for stain removal
Peroxide toothpastes for gentle brightening
(Professional whitening for bigger shade changes)For ingredient sensitivities or frequent ulcers:
SLS free toothpasteDuring chemotherapy or if your mouth feels sore and delicate:
SLS free, mild flavour toothpaste and a soft brush
If you are ever unsure what is right for your mouth, speaking to a dental professional is the safest place to start.
About the Author
Colette Lawler is a UK based dental hygienist and therapist and freelance medical writer. She specialises in oral health, oral cancer awareness, and digital health communication, with a focus on turning complex science into clear, practical advice.
Welcome to ByteWise: Where Oral Health, Digital Health and Human Stories Meet
ByteWise is here — a space where oral health, digital health and human stories meet. In this first post, I share why the mouth matters more than people realise, how it connects to whole-body health, and what you can expect from the ByteWise community moving forward.
I’m so glad you’re here.
If we haven’t crossed paths properly yet, I’m Colette — a dental clinician turned medical writer who’s spent more than twenty years watching how the mouth quietly reflects what’s happening elsewhere in the body. Sometimes long before anyone thinks to connect the dots.
When I’m not in clinic or writing, I’m juggling three kids, a husband on brutal shifts, and a sprocker who’s made off with more shoes than I care to admit. Real life is beautifully chaotic… and if I’m honest, it sparks half my ideas.
Because through all of it, one thing has stayed constant: curiosity.
Curiosity about patterns, early clues, and the quiet ways oral health mirrors whole-body health.
ByteWise has been brewing for a while, and this blog — alongside my newsletter — is my way of bringing that curiosity to life. Think of it as a place where we explore how the mouth, the body and technology are far more connected than most people realise.
Why Start ByteWise Now?
Because oral health is still treated like a side mission in the bigger health conversation.
And it shouldn’t be.
Your mouth reacts to hormones.
It mirrors inflammation.
It often changes before the rest of your body sends clearer signals.
Yet despite all this, oral health is almost entirely missing from digital-health tools — even though it’s one of the most powerful early indicators we have.
ByteWise exists to help change that: gently, clearly, and with a bit of personality along the way.
If you’re curious about how oral health fits into the bigger picture — hormones, chronic disease, AI, digital tools and everything in between — you’ll feel right at home here.
What You Can Expect from ByteWise
🧠 Insightful, research-backed micro deep dives
Exploring the fascinating, often-overlooked ways the mouth connects with the rest of the body.
📘 Smart, digestible explainers
Clear, human explanations without the jargon overload.
🩺 Real clinical stories & honest reflections
Two decades in the treatment room have taught me a lot about people, patterns and the power of early detection.
💡 Digital tools worth knowing about
Wearables, apps, AI, emerging salivary tech — the tools that genuinely support health, not overwhelm it.
✨ Practical, everyday insights
Small things you can look for that make a real difference to comfort, confidence and whole-body health.
Why This Matters
The mouth is still the missing data layer in so many areas of healthcare — women’s health, cardiovascular disease, diabetes, mental health.
And now, with AI, biomarkers and smart sensors evolving rapidly, we’re entering a new era of connected health.
But technology is only useful if people understand it.
That’s where clear, human communication comes in — and that’s what ByteWise is here to offer.
Who This Blog Is For
Clinicians, writers, founders, women’s-health advocates, digital-health thinkers — and anyone who simply wants to understand their body a little better.
If you’re curious, this space will feel like home.
A Quick Promise from Me
Everything you find here will be:
Clear
Warm
Evidence-based
Grounded in real clinical experience
Free from hype, gimmicks and unnecessary drama
Written with the same honesty and care I bring to my clinical work.
Coming Up Next: Inside Your Toothpaste
The next post takes you behind the scenes of toothpaste ingredients — what actually protects your teeth, what doesn’t, and why the formula matters more than the flavour.
Thank you for being here.
Let’s grow this ByteWise community together.
Colette x