Why health advice doesn’t stick — and what oral health can teach us about making habits easier
Health advice doesn’t fail because people don’t care. It fails because real life creates friction. Here’s what oral health can teach us about designing habits that actually stick — with clearer priorities, better prompts, and more supportive systems.
January is peak “new habits” season.
And yet, every year, many of those habits quietly fade — not because people don’t care, but because real life gets in the way.
In oral health, I see this all the time.
I’m Colette — a UK-based dental clinician and medical writer — and I spend a lot of time thinking about the overlap between oral health, prevention, and the systems (and tech) that make healthy habits easier to stick to.
Because advice can be clinically spot-on… and still not stick.
In clinic, it’s often clear that knowledge isn’t the missing piece. Many patients already know the basics: brush twice a day, clean between teeth, watch the sugar.
And yet, a patient said to me recently:
“I know what I’m meant to do… I just don’t manage it.”
That gap — between knowing and doing — is where prevention often breaks down.
And it’s why motivation alone is rarely the answer.
Why health advice doesn’t stick (even when it’s correct)
Most oral health (and general health) advice is well-intentioned and evidence-based.
But behaviour doesn’t happen in ideal conditions. It happens on busy mornings, late nights, shift patterns, school runs, sensory overload days, anxious days, and the “I’ve got nothing left in the tank” days.
So when habits slip, it’s rarely because someone doesn’t care.
More often, it’s because the habit sits behind too much friction.
Common reasons health habits fail (the friction points)
Too much complexity
Too many products, too many claims, too many “rules”. When people feel confused, they often do nothing.
No clear priority
If everything sounds equally important, it’s hard to know what matters today.
Timing
Advice is often given at a moment when people can’t act. The moment passes, and life takes over.
Shame and self-judgement
If someone feels they’ve already “failed”, they avoid the topic altogether. Shame doesn’t build habits — it blocks them.
Life factors that don’t get acknowledged
Neurodivergence, anxiety, depression, medication-related dry mouth, chronic illness, caring responsibilities, cost. These aren’t edge cases — they’re real life.
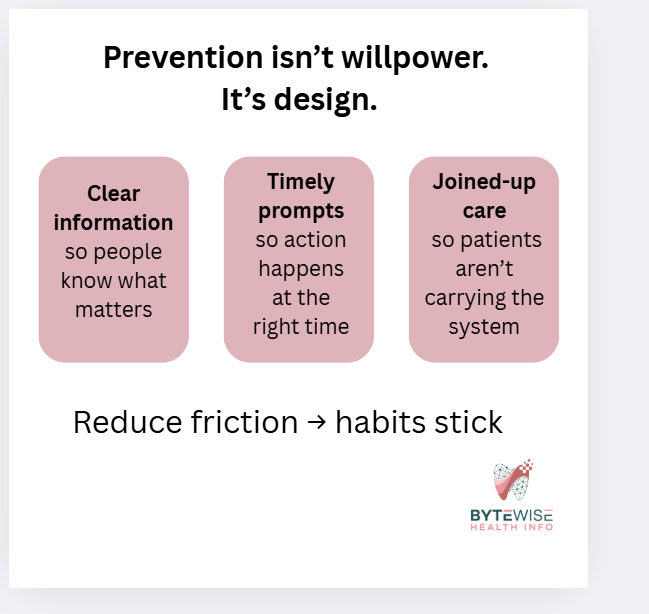
This is why I keep coming back to a simple idea:
Prevention is easier when the system is designed to support it — not with more pressure, but with better support.
Knowing vs doing: where prevention really lives
Most prevention challenges sit in the gap between:
Capability — Do I know how? Do I have the tools?
Opportunity — Is my environment set up to help me?
Motivation — Do I want to do this, and does it feel worth it?
We often focus heavily on motivation: try harder, be consistent.
But opportunity is frequently the missing piece — the prompts, routines, environment, and joined-up care that make follow-through more likely.
This is also where digital tools can help — including reminders, smart prompts, and in some cases wearables — as long as they’re designed around real human behaviour, not perfect routines.
What better systems (and tech) could do
This isn’t about fancy gadgets or downloading yet another app that gets abandoned by Thursday.
It’s about reducing friction and making prevention easier to repeat.
1. Personalised prevention, not one-size-fits-all
Oral health advice is often generic — but people aren’t.
Someone with dry mouth, braces, diabetes risk, previous gum disease, or high sugar exposure needs different support from someone who’s low risk.
Better systems could translate risk into clear, usable guidance like:
“Here are your top two priorities this month.”
“Here’s the one habit that will give you the biggest win.”
“Here’s what to focus on until your next visit.”
Clarity reduces overwhelm.
2. Prompts at the right moment (not random reminders)
Most reminders fail because they arrive when you can’t act.
More effective prompts show up at the point of decision — when a routine is already happening.
Even low-tech prompts work well:
linking interdental cleaning to an existing habit
keeping brushes or floss where you actually sit
a simple routine card on the bathroom mirror
recall messages sent during opening hours, when booking is easy
Tech can help with timing — but the goal is simple: make the next right action easier.
3. Joined-up records that support joined-up care
Oral health is linked to systemic health, medication, pregnancy, and chronic conditions — yet records are often siloed. This is something I explore further in my white paper on integrating dental and medical health records.
When data isn’t joined up, we rely on:
patients repeating their story
memory (not a safe clinical tool)
missed prevention opportunities
Better integration could flag:
diabetes risk and gum inflammation
medication-related dry mouth
anticoagulants and dental planning
osteoporosis medications
pregnancy-related inflammatory windows
This isn’t about “more data”.
It’s about the system doing some of the heavy lifting — so patients don’t have to.
4. Prevention that continues between appointments
Most people see a dental professional occasionally — but habits are daily.
Systems and tech could help bridge that gap with:
simple check-ins
consistent, non-judgemental encouragement
short, personalised “next step” nudges
easy access to the right education at the right time
Prevention works best when it feels supported, not like a once-a-year reset.
Three tiny friction-reducers to try this week
You don’t need a personality transplant. You need a simpler setup.
1. Put tools where the habit actually happens
Out of sight = out of routine. Move tools to where you intend to use them and leave them on show.
2. Attach the habit to something you already do
Borrow an existing routine so you don’t rely on memory.
3. Shrink the task
A “minimum version” still counts. Consistency beats perfection.
A quick note on shame
If you’ve ever felt embarrassed about your oral health routine, you’re not alone.
But shame doesn’t create good habits.
It creates avoidance.
Better systems support people — they don’t judge them.
Where I’m going with this in 2026
This year I’m leaning further into the systems side of prevention.
Not just what we tell people to do — but what actually helps people do it, consistently, in real life.
That includes:
clearer risk communication
better-timed prompts
joined-up records
and tech that supports habits without adding guilt
I’m also starting a behaviour change course to strengthen this side of my work — so my content is not only clinically accurate, but genuinely usable.
One last question
What’s the biggest thing that gets in the way of oral health habits sticking — for you, or for your patients?
Forgetfulness?
Time?
Anxiety or sensory issues?
Cost or access?
Medication or health factors?
Or just… life?
These real-world barriers are where better prevention design starts.